The diagnosis of TBI, especially mild TBI, is essentially a clinical diagnosis. There is no single specific testing to be purely diagnostic for mild TBI at this point. Currently we use Neurological and a variety of imaging studies to make this diagnosis
There are two types of neurologic tests: those that examine the structure of the brain and those that examine the function of the brain. The CAT scan and MRI look at the structure of the brain. The electroencephalogram (EEG), SPECT scan, PET scan, and evoked studies examine the function of the brain.
The 3 Tesla MRI and CAT scan, slice the brain radiographically into thin layers. The MRI does this with magnetic fields and the CAT scan uses x-rays. The MRI provides more detail than the CAT scan. Hence, brain damage seen on an MRI – as small as 1-2mm in size — may escape detection by a CAT scan. The CAT scan is superior to the MRI in detecting fresh blood in and around the brain, while the MRI is better at detecting the remnants of old hemorrhaged blood, called hemosiderin.
This is a software program which enables an MRI to more accurately show tiny hemorrhages known as microhemorrhages. These small white dots actually show up on the MRI because of the iron content left behind after blood has been in an area through injury. These tiny capillaries in the brain are torn and the small amounts of blood can be seen on SWI-MR. In persons fifty or older, there are white dots, which can often be from aging. In the younger person, or in an older person where these abnormalities are clustered at the grey-white junction (where the grey matter meets the white matter) are generally traumatically caused. There can be as many as several hundred of these small injuries throughout the brain, but they are an objective unarguable type of evidence for brain injury and are exceedingly helpful in any brain injury litigation. They can also identify the areas of the brain that have been shaken and can aid in rehabilitative strategies.
Diffusion Tensor Imaging is a type of MRI which uses special software to view parts of the brain a normal MRI cannot. The interesting premise of this new technology is that it measures the movement of water molecules in relation to the white track fibers of the white matter of the brain. If the fibers are healthy and untorn, then the water molecules will show parallel movement along those tracks as they slide along them. Torn or missing white matter fiber will allow perpendicular movement of the water molecules.
This new technology allows for visualization of natural damage to the white matter. It is a very impressive technology and will be impressive to jurors and others involved in TBI litigation. Most radiology groups do not have this software, so if you would like to have this test run, try University centers first. DTI will be especially helpful in cases involving high velocity change injury, such as high speed car accidents, falls from a height, and other accidents in which the injury is suspected to be Diffused Axonal Injury (DAI).
Monitors the brain’s electrical activity by means of wires attached to the patient’s scalp. These wires act like an antenna to record the brain’s electrical activity. Any underlying damage can cause slowing in the electrical activity or abnormal discharges which are called spikes or sharps (seizure activity).
This test is performed in a way similar to EEG. Brain wave activity varies throughout the day depending on the state of alertness. Brain mapping computers are now capable of creating a map of the brain’s electrical activity depicting how long each area of the brain spends in each of the basic rhythms. By comparing the patient’s map with that of a control population, it is possible to localize areas of focal slowing of electrical activity. Alone, a QEEG is insufficient to diagnose brain damage but in conjunction with other neurologic tests, QEEG can be confirmatory.
PET scanning (positron emission tomography) is based on the fact that the brain uses glucose for energy. By labeling a glucose molecule with a radioactive “tag,” and then inhaling radioactive glucose, one can identify abnormal areas of the brain that are underutilizing glucose. Because cyclotrons are needed to generate the radioactive gas, PET scanning is not widely available.
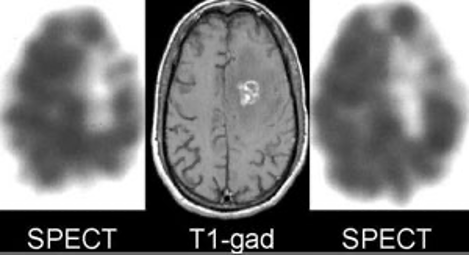
SPECT scanning (single photon emission computed tomography) is similar to PET scanning in that a radioactive chemical is administered intravenously to the patient, but the radioactive chemical remains in the bloodstream and does not enter the brain. As a result, the SPECT scan maps the brain’s vascular supply. Because damaged brain tissue normally shuts down its own blood supply, focal vascular defects on a SPECT scan are circumstantial evidence of brain damage. The advantage of a SPECT scan over a PET scan is its ready availability and relatively cheap cost. Recent studies have demonstrated abnormal SPECT scans after head trauma when the CAT and MRI were normal, suggesting that the SPECT scan is more sensitive to brain injury then either CT or MRI scans. Because the radioactive chemicals used in SPECT and PET scans are carried to all parts of the body by vascular tree.
Evoked studies take advantage of the fact that each time a sensory system of the body — vision, hearing, touch — is stimulated, an electrical signal is generated in the brain. These electrical signals can be detected with electrical wires on the scalp. Thus, visual evoked recordings (VER) are recorded over the occipital lobes; brainstem auditory evoked recordings (BAER) over the temporal lobes; and somatosensory potentials (SSEP) over the parietal lobes.
This is an exciting new tool, used in conjunction with MRI, that detects the intra-cellular relationship of brain metabolites. Studies show that in an injured brain, the relationship between the amount of certain compounds in the brain changes in predictable ways, which can be picked up, non-invasively, by MRS. While MRS is in its early stages, it holds great promise in the “objectivication” of brain injury. THIS DATA CAN AND SHOULD BE CAPTURED ON MRI WITHIN SIX WEEKS OF INJURY.


Dr. Amirhassan Bahreman is the director of Neurological and Pain Institute, Inc., San Diego's leading expert on traumatic brain injury (TBI) and other neurological conditions.
8851 Center Dr., Ste 608
La Mesa, CA 91942
619-460-5850
619-460-5849 (FAX)
Website by SRL Group - Copyright © 2020 Dr. Amirhassan Bahreman